Physiologic jaundice of the newborn (hyperbilirubinemia) is the most common type of jaundice. All newborns have some elevation of bilirubin in the first week of life compared to adult levels because newborns have an immature liver and gastrointestinal tract. The most common cause of jaundice for term newborns occurring in the first week of life is associated with not getting enough milk at the breast. Dehydration and ongoing weight loss occur.
Small quantities of colostrum are appropriate for the size of a newborn’s stomach. A one-day-old newborn has a stomach size of a cherry and may receive no more than 5 mL (a teaspoon) at each breastfeeding. Newborns need to breastfeed approximately 8-10 times in 24 hours. In the first week of life, the newborn’s stomach size changes, and the amount of milk intake increases as colostrum changes to mature milk. A three-day-old newborn has the stomach size of a walnut and needs to take approximately 1 oz at each breastfeeding. At 5-7 days of age, infants need to take 1-1/2 to 2 oz per breastfeeding. A newborn with ongoing weight loss is probably associated with a lack of these increasing milk intakes.

Mothers and Infants at Risk for Jaundice include:
- Preterm infants born < 36 weeks gestation
- Near term infants born between 36-38 weeks gestation
- Bruising or cephalohematoma
- Poor feedings – newborn sleepy at breast
- Weight loss >10% of birthweight
- Delay in passing meconium stool
- Maternal diabetes or gestational diabetes
- ABO incompatibility
- Having a prior newborn with jaundice
The above factors can contribute to developing jaundice and to a low milk supply. However, most moms and babies can continue to breastfeed successfully when given appropriate assessment of the condition, evidence-based interventions, and ongoing evaluation of progress until adequate weight gain is achieved by taking enough milk when breastfeeding.
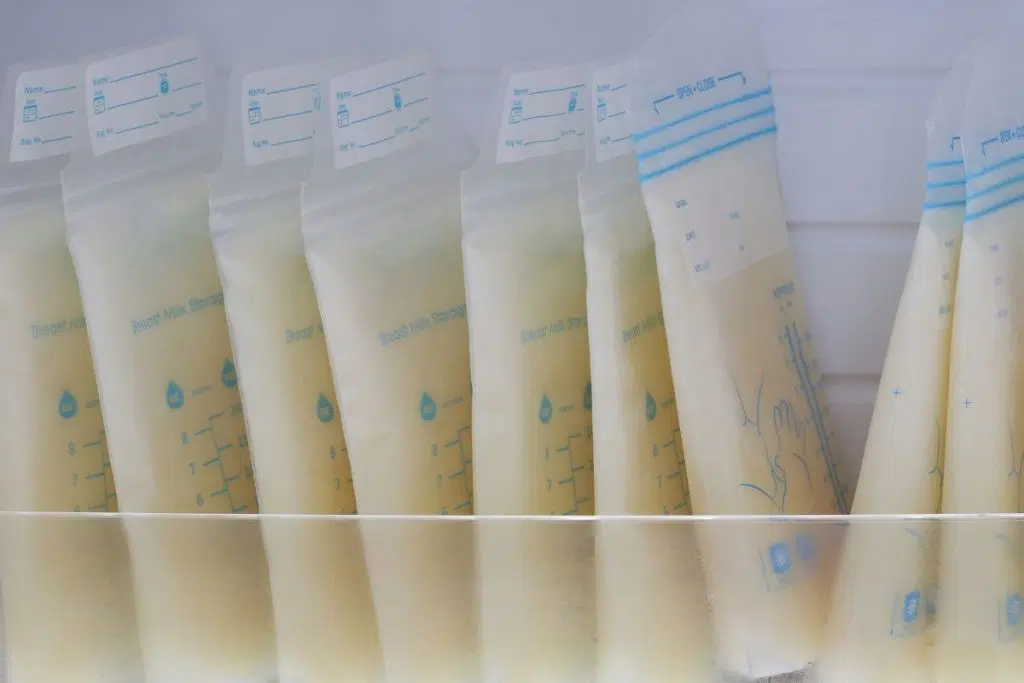
Your newborn physician’s management of jaundice may include monitoring of bilirubin levels, phototherapy, and continuation of breastfeeding with additional feedings for hydration and weight gain such as your pumped breastmilk, donor milk, or formula.
My role is to assist with latching technique, to monitor intake at breast using the Medela BabyWeigh Scale, and to establish a feeding and pumping plan. Research findings support the use of the Medela Symphony pump to Initiate and Maintain an adequate milk supply. I will teach you how to properly use the breast pump. Most moms can make enough milk for their baby. Send me an email or give me a call. I provide these guidelines for managing this problem while recognizing the need for adjusting the guidelines to the individual needs of each infant.